At Home Sleep Study — Complete Guide to Testing Sleep Disorders from Home
Introduction
Sleep has become one of the most talked-about health topics in recent years — and for good reason. With more than 70 million Americans affected by sleep disorders and millions more worldwide struggling with poor-quality rest, the demand for easier, faster, and more affordable diagnostic options is on the rise. This growing awareness has fueled the popularity of at home sleep studies, a modern alternative to traditional hospital or lab-based tests.
So, what exactly is an at home sleep study?
In simple terms, it’s a sleep test you can do in your own bedroom, using a small portable device that records your breathing, oxygen levels, heart rate, and other signals while you sleep. Instead of spending the night in a hospital hooked up to dozens of wires, you’re able to monitor your sleep health comfortably from home — often with the same level of accuracy for common conditions like obstructive sleep apnea (OSA).
Compared to a traditional sleep lab (also called polysomnography), at-home sleep studies are:
- More convenient — you sleep in your own bed.
- More affordable — typically a fraction of the cost of an in-lab test.
- Less comprehensive — they focus mainly on diagnosing sleep apnea rather than complex conditions like narcolepsy or REM behavior disorder.
Why does this matter? Because sleep problems are no longer rare or minor inconveniences. Rates of sleep apnea, chronic insomnia, and restless sleep are increasing worldwide, with links to serious health risks such as high blood pressure, diabetes, heart disease, and even reduced workplace performance. Catching these conditions early — without the barrier of hospital visits or high costs — can make the difference between living tired and living well.
An at home sleep study bridges the gap by making sleep testing more accessible, efficient, and patient-friendly — helping more people take control of their sleep health without stepping outside their front door.
What Is an At Home Sleep Study?
An at home sleep study (often called a home sleep apnea test or HSAT) is a diagnostic test you take in the comfort of your own home to monitor sleep patterns, breathing, oxygen levels, and heart activity. Unlike a full overnight sleep lab test, which requires spending the night in a clinic, an at home sleep study uses a portable sleep monitor with lightweight sensors to collect data while you sleep in your own bed.
How It Works
- Setup: Your doctor or provider sends you a portable device with simple instructions.
- Sensors: The kit usually includes a nasal cannula (to measure airflow), a chest belt (to track breathing effort), and a fingertip sensor (to measure blood oxygen).
- Recording: As you sleep, the device records data on breathing pauses, snoring intensity, oxygen drops, and heart rate.
- Review: In the morning, the results are uploaded (manually or via Bluetooth) and analyzed by a sleep specialist.
This streamlined process is particularly effective for diagnosing obstructive sleep apnea (OSA), one of the most common sleep disorders.
Polysomnography vs. HSAT
- Polysomnography (PSG): A comprehensive in-lab sleep test that monitors brain waves, eye movement, muscle activity, heart rhythm, and more. It’s used to diagnose a wide range of sleep disorders, including narcolepsy and parasomnias.
- Home Sleep Apnea Test (HSAT): A simplified version done at home. It primarily focuses on sleep-disordered breathing (like sleep apnea) but doesn’t capture the full spectrum of sleep-related conditions.
In short:
- Polysomnography = Gold standard for complex cases
- HSAT = Convenient, affordable option for suspected sleep apnea
Polysomnography vs. Home Sleep Apnea Test (HSAT)
- Polysomnography (PSG):
- HSAT (Home Sleep Apnea Test):
👉 In short: Polysomnography = full in-lab test for complex conditions, while HSAT = convenient at-home test for suspected sleep apnea.
Why Choose an At Home Sleep Study?
When deciding whether to test your sleep health at home or in a clinic, the advantages of an at home sleep study often stand out. From convenience to affordability, this option is designed for people who want reliable answers without unnecessary stress or costs.
Convenience and Comfort
One of the biggest reasons people choose at home testing is comfort. Instead of sleeping in a hospital or clinical setting—surrounded by wires, monitors, and unfamiliar noises—you simply rest in your own bed, in your own environment. This makes the results more natural, since your sleep isn’t disrupted by an unfamiliar space.
- No travel required: You don’t need to drive to a hospital or clinic for an overnight stay.
- No overnight disruption: The test works around your normal bedtime routine, making the experience less stressful.
- More natural sleep patterns: Sleeping at home gives a more accurate picture of how you actually sleep every night.
Cost and Accessibility
Another advantage of home testing is affordability. Traditional lab-based polysomnography can cost over $1,000 to $3,000 per night, while most at home sleep studies range from $150 to $500, depending on the provider.
- Lower out-of-pocket costs: At home studies are typically a fraction of the price of lab studies.
- Insurance coverage: Many health insurance plans, including Medicare and private insurers, now cover at home sleep apnea tests if ordered by a physician. Always check with your provider before scheduling.
- Greater access: Telehealth services and mail-order kits have made it easier for patients in rural or underserved areas to get tested without traveling long distances.
Accuracy and Limitations
While an at home sleep apnea test (HSAT) is highly effective for diagnosing obstructive sleep apnea (OSA), it does have its limitations.
- Reliable for OSA diagnosis: Multiple studies have shown that HSATs are comparable to lab studies when it comes to detecting moderate to severe sleep apnea.
- Limited for complex disorders: Because HSATs focus mainly on breathing patterns, they may not capture other sleep disorders such as narcolepsy, parasomnia, periodic limb movement disorder, or REM behavior disorder. For these conditions, a full in-lab polysomnography is still necessary.
- Device setup matters: If sensors are attached incorrectly, results may be inconclusive or require retesting.
◆Pull Quote: “At-home sleep studies are best for diagnosing obstructive sleep apnea, not all sleep disorders.”
Who Should Consider an At Home Sleep Study?
An at home sleep study isn’t for everyone, but it can be the right choice for people who show signs of obstructive sleep apnea (OSA) or who are at higher risk of developing sleep-related breathing disorders. Doctors often recommend this option when symptoms are clear and a simpler, more cost-effective test can provide reliable results.
People with Suspected Sleep Apnea
If you experience any of the following, a home sleep study may help:
- Loud, chronic snoring
- Pauses in breathing during sleep (often noticed by a partner)
- Daytime fatigue or morning headaches despite getting enough hours of sleep
- Difficulty concentrating or irritability due to poor-quality rest
These symptoms are strongly associated with sleep apnea, the condition most commonly diagnosed through at home testing.
High-Risk Groups
Certain health conditions make sleep apnea more likely. You should consider an at home sleep study if you fall into any of these categories:
- Obesity: Excess weight increases the risk of airway obstruction.
- High blood pressure (hypertension): OSA is closely linked to resistant hypertension.
- Type 2 diabetes: Many people with diabetes also have undiagnosed sleep apnea.
- Family history of sleep apnea: Genetics can increase your likelihood.
- Lifestyle factors: Smoking, alcohol use, and sedentary habits can worsen sleep quality.
Patients Recommended by Sleep Specialists
In many cases, a sleep physician will suggest an at home sleep study after an initial consultation. This is especially true if:
- Your symptoms strongly suggest sleep apnea.
- You have no other major sleep disorders suspected.
- You prefer a less invasive, more accessible testing option.
Self-Check Quiz — Do I Need a Sleep Study?
Answer Yes or No to the following:
- Do you snore loudly or regularly disturb your partner’s sleep?
- Has anyone noticed you stop breathing during sleep?
- Do you often feel excessively tired during the day, even after 7–8 hours of sleep?
- Do you wake up with headaches, dry mouth, or a sore throat?
- Do you have high blood pressure, diabetes, or obesity?
- Do you struggle with focus, memory, or mood swings due to poor rest?
👉 If you answered “Yes” to 2 or more, it may be time to talk to your doctor about an at home sleep study.
How Does an At Home Sleep Study Work?
An at home sleep study may sound complex, but the process is straightforward and designed for ease of use. Most patients complete the test in a single night without disruption to their normal sleep routine.
Step-by-Step Process
Doctor Consultation & Prescription
- Most at home sleep studies begin with a consultation. A primary care doctor or sleep specialist will review your symptoms—such as snoring, fatigue, or breathing pauses—and determine if a home test is appropriate.
- In many regions, a doctor’s order is required before a home sleep study can be issued, especially if insurance coverage is involved.
Device Setup Instructions
- You’ll receive a portable testing kit either by mail or directly from a sleep clinic.
- The kit comes with step-by-step instructions, often supported by video tutorials or a phone call from a technician.
- Most devices are designed for simple, do-it-yourself setup, with color-coded parts and minimal wires.
Overnight Test at Home
- On the night of your test, you’ll wear a few lightweight sensors while you sleep in your own bed.
- The device records data such as airflow, oxygen levels, breathing effort, heart rate, and snoring intensity.
- Unlike in-lab studies, you won’t be observed—everything happens naturally in your regular sleep environment.
Data Upload & Physician Review
- The next morning, you’ll return the device (or sync it via Bluetooth/Wi-Fi, depending on the model).
- The recorded data is analyzed by a sleep physician, who generates a detailed report.
- You’ll then discuss results and treatment options, such as CPAP therapy, oral appliances, or further testing if needed.
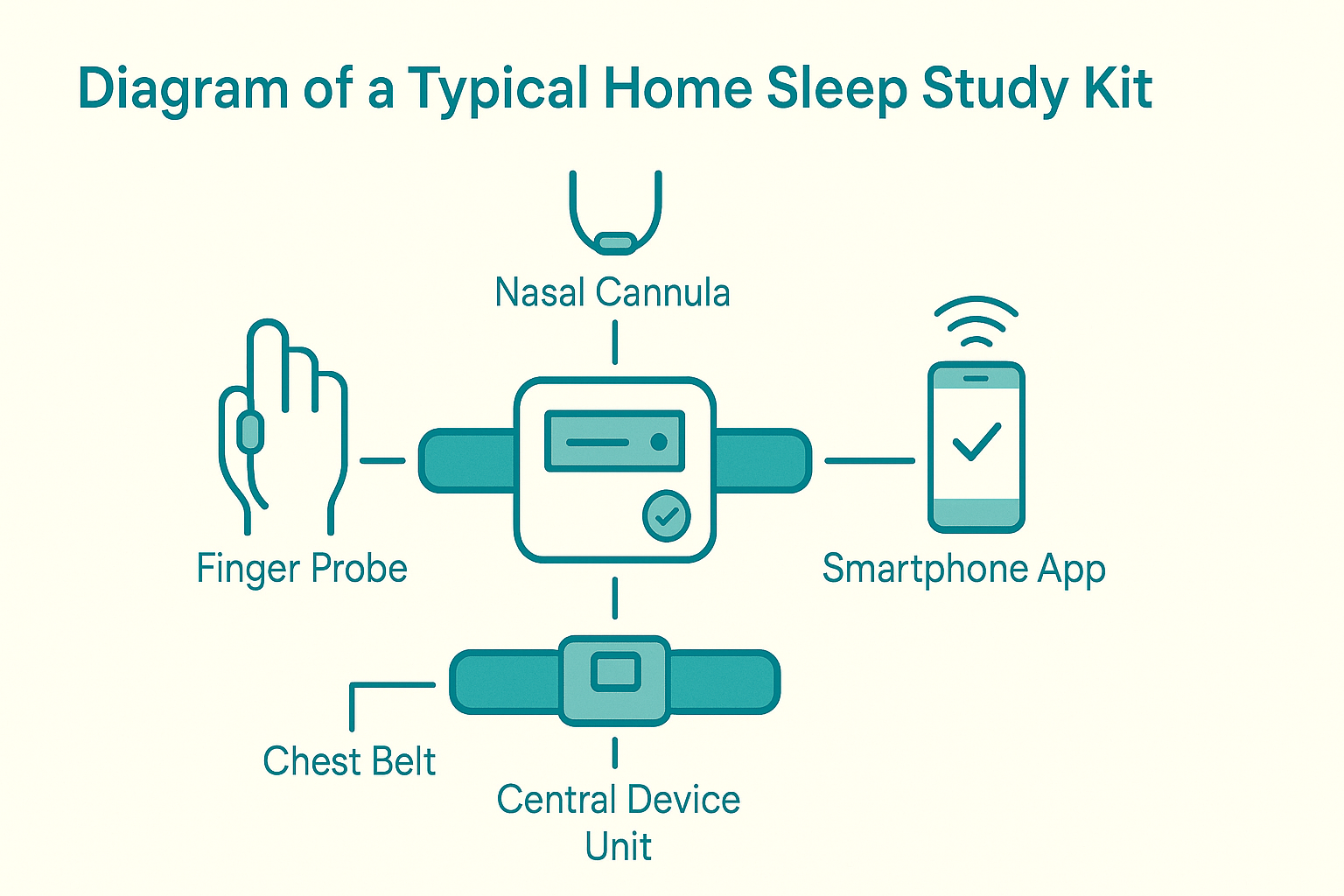
Equipment Used in Home Sleep Studies
While equipment varies by provider, most home sleep apnea test kits include three core sensors:
- Breathing Sensor (Nasal Cannula): Tracks airflow through your nose and mouth to detect pauses or reductions in breathing.
- Oxygen Saturation Monitor (Pulse Oximeter): Usually placed on your finger, it measures oxygen levels in your blood and pulse rate throughout the night.
- Chest or Abdomen Belt: Records breathing effort and movement of the chest or stomach to identify respiratory patterns.
Some modern app-based devices go a step further:
- Bluetooth or Wi-Fi connectivity for automatic uploads.
- Smartphone apps with guided setup and troubleshooting.
- Real-time feedback on sensor placement and recording quality.
These innovations make home sleep studies more user-friendly and reduce the likelihood of inconclusive results.
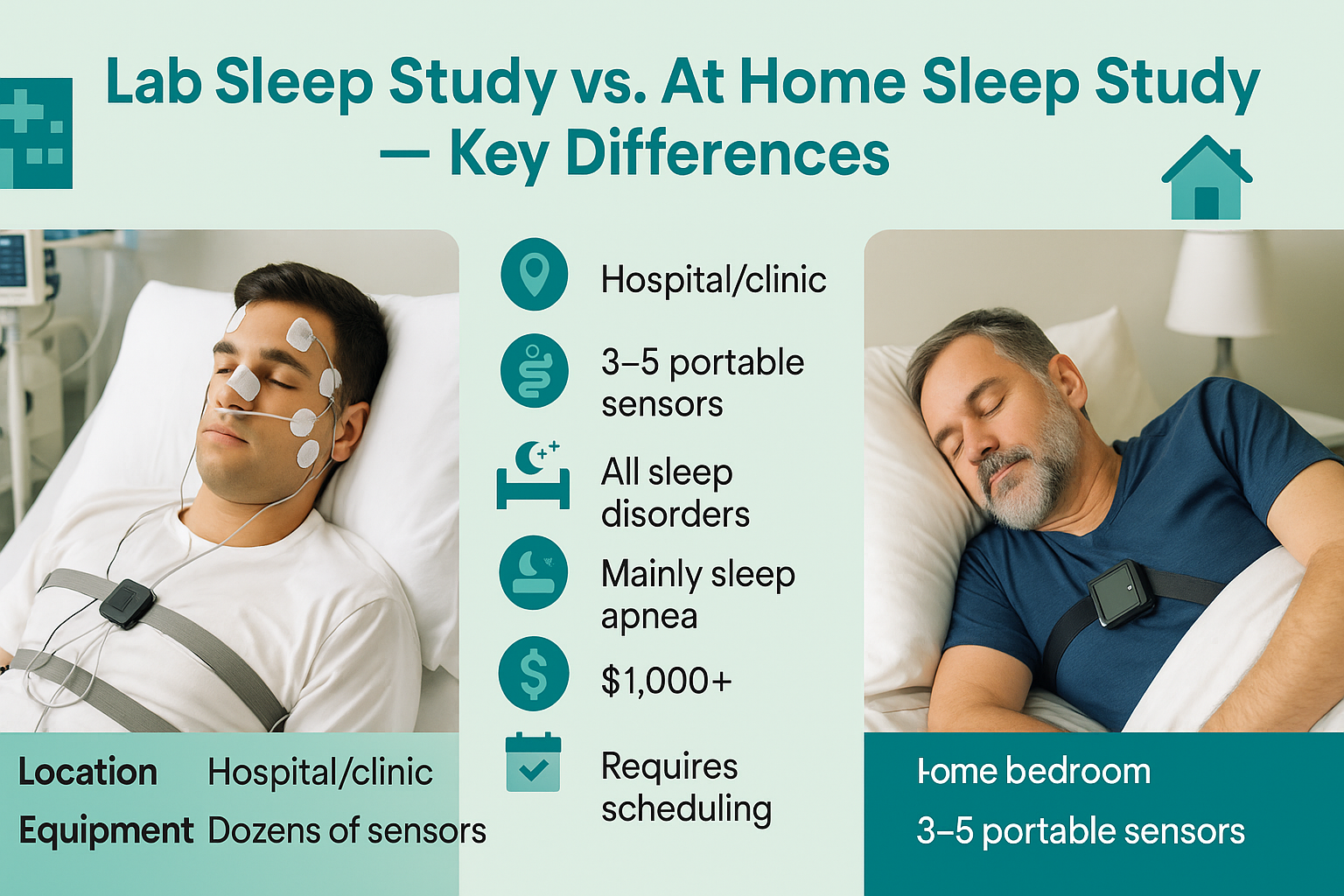
At Home Sleep Study vs. In-Lab Sleep Study
When it comes to diagnosing sleep disorders, patients are often presented with two main options: at-home sleep studies (HSAT – Home Sleep Apnea Testing) and in-lab polysomnography (PSG). While both approaches are designed to evaluate sleep patterns and detect issues such as sleep apnea, they differ significantly in accuracy, cost, comfort, and the complexity of conditions they can diagnose.
Understanding these differences can help you decide which type of study best fits your health needs, lifestyle, and budget.
Side-by-Side Comparison: HSAT vs. In-Lab Polysomnography
| Feature | At-Home Sleep Study (HSAT) | In-Lab Sleep Study (Polysomnography) |
|---|---|---|
| Accuracy | Good for detecting moderate to severe obstructive sleep apnea (OSA). May miss mild cases or other sleep disorders. | Gold standard for sleep diagnostics. Measures brain activity (EEG), eye movement, muscle tone, heart rhythm, oxygen levels, and breathing. |
| Cost | Generally lower ($150–$500, depending on provider). Often covered by insurance. | Higher cost ($1,000–$3,000+). Insurance may cover with physician referral. |
| Comfort | Conducted in your own bed, natural sleep environment, less intimidating. | Conducted in a sleep lab/clinic. Monitors and sensors may feel uncomfortable or disrupt sleep. |
| Complexity of Disorders Diagnosed | Primarily screens for sleep apnea and related breathing disorders. Limited scope. | Can diagnose a wide range of sleep disorders (e.g., insomnia, narcolepsy, REM behavior disorder, restless legs syndrome). |
| Convenience | Simple setup, fewer sensors, no need to travel. | Requires overnight stay in a sleep lab, monitored by technicians. |
| Monitoring Support | No live technician support during the test. | Continuous monitoring by trained sleep technicians. |
| Results Turnaround | Usually available within a few days. | May take longer due to more complex data analysis. |
HSAT Differences vs. In-Lab Polysomnography
- HSAT (Home Sleep Apnea Testing) is best suited for patients who are suspected to have moderate to severe sleep apnea and prefer convenience and affordability.
- In-lab polysomnography, on the other hand, is the gold standard for comprehensive evaluation, capable of diagnosing a wide spectrum of sleep disorders—not just apnea.
- Doctors often recommend starting with HSAT when symptoms strongly suggest obstructive sleep apnea. However, if results are inconclusive or if another disorder is suspected, an in-lab test is usually the next step.
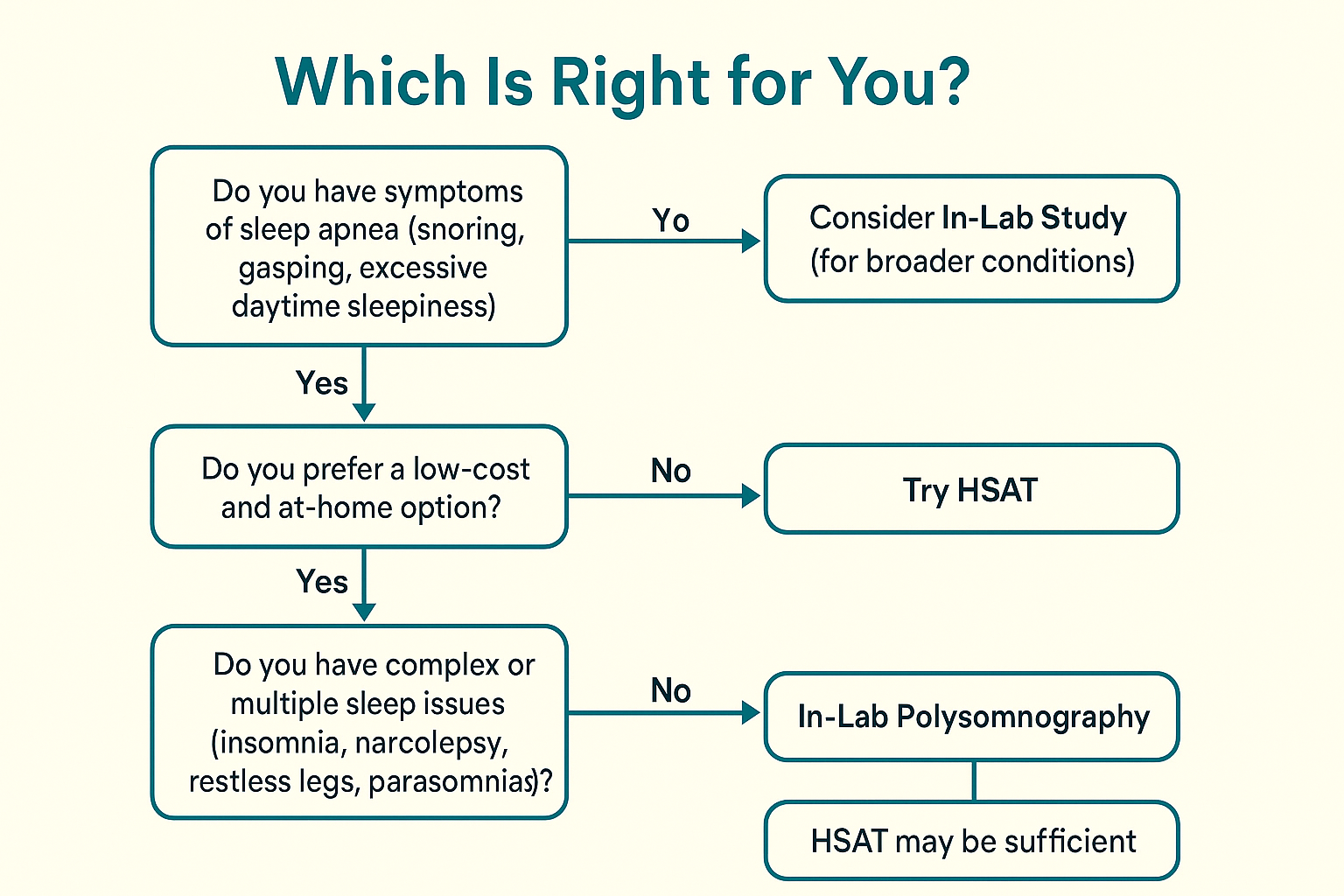
👉 Key takeaway: If you’re looking for convenience and cost-effectiveness, an at-home sleep study might be right for you. But if you need a comprehensive and highly accurate diagnosis, especially for complex sleep conditions, in-lab polysomnography is the gold standard.
Preparing for Your At Home Sleep Study
An at-home sleep study (HSAT) is designed to be simple and stress-free, but preparing properly can make a big difference in the accuracy of your results. Following these steps will help ensure the test reflects your natural sleep patterns.
1. Avoid Caffeine and Alcohol Before the Test
- Caffeine (coffee, tea, soda, energy drinks) can interfere with your ability to fall asleep and may alter breathing patterns.
- Alcohol may make you drowsy at first, but it disrupts normal sleep stages and can mask or worsen breathing issues like sleep apnea.
- Tip: Avoid both for at least 6–8 hours before your test.
2. Follow Your Regular Bedtime Routine
- Go to bed at your normal sleep time—this ensures the test reflects your usual sleep behavior.
- Brush your teeth, read, or relax as you normally would.
- Avoid starting new habits (like exercising late or taking unfamiliar sleep aids) that could affect results.
3. How to Properly Wear Sensors
- Most HSAT devices include sensors for your finger (oxygen levels), nose (airflow), and chest/abdomen (breathing effort).
- Follow your provider’s instructions carefully when attaching sensors.
- Make sure straps are snug but not too tight—comfortable enough to sleep in.
- Double-check that lights or indicators on the device show it’s working before you lie down.
Tip Pull-Out: Checklist – Do’s & Don’ts Before Your Sleep Study
✅ Do’s
- Go to bed at your usual time
- Charge or prepare the device in advance
- Wear loose, comfortable sleepwear
- Attach sensors as instructed
- Sleep in your normal position (back, side, etc.)
❌ Don’ts
- Don’t consume caffeine or alcohol within 6–8 hours of bedtime
- Don’t take naps during the day (unless directed by your doctor)
- Don’t apply lotions or oils on your chest/face (can interfere with sensors)
- Don’t worry if you wake up at night—just go back to sleep naturally
👉 Key takeaway: Treat the study night like any other night, with just a few extra steps to set up the equipment. A calm, normal routine will give your sleep specialist the clearest picture of your natural sleep patterns.
Understanding Your At Home Sleep Study Results
Completing your at-home sleep study is only the first step. The real value comes when your doctor interprets the data to determine whether you have a sleep disorder like obstructive sleep apnea (OSA) and what treatment might help.
Key Terms You’ll See in Your Results
AHI (Apnea-Hypopnea Index):
- The number of times per hour your breathing stops (apnea) or becomes shallow (hypopnea).
- Severity levels:
→ Mild: 5–14 events/hour
→ Moderate: 15–29 events/hour
→ Severe: 30+ events/hour
Oxygen Desaturation:
- Refers to drops in blood oxygen levels during sleep.
- Frequent or significant desaturations indicate your body isn’t getting enough oxygen at night.
Sleep Efficiency:
- The percentage of time spent asleep vs. time spent in bed.
- Lower efficiency can point to insomnia or frequent awakenings.
How Doctors Interpret Your Results
A sleep specialist looks at more than just raw numbers:
- Pattern of Events: Are breathing interruptions clustered or spread out?
- Position Dependence: Do events worsen when you sleep on your back?
- Severity of Oxygen Drops: How low did oxygen saturation go, and for how long?
- Symptoms + Data: Results are compared with your reported symptoms (daytime sleepiness, snoring, morning headaches) for a full picture.
Next Steps After Your Sleep Study
- CPAP (Continuous Positive Airway Pressure): The most common treatment for moderate to severe sleep apnea. It delivers gentle air pressure through a mask to keep airways open.
- Lifestyle Changes: Weight loss, avoiding alcohol before bed, adjusting sleep position, and improving sleep hygiene can reduce symptoms.
- Oral Appliances: For mild to moderate cases, dentists may fit devices that keep the airway open by repositioning the jaw.
- Further Testing: If your results suggest complex sleep disorders (like narcolepsy or parasomnia), an in-lab polysomnography may be required for more detailed monitoring.
👉 Key takeaway: Your at-home sleep study provides critical insights, but only a licensed healthcare provider can interpret the results and recommend the right treatment plan tailored to you.
Benefits and Drawbacks of At Home Sleep Studies
Like any medical test, at-home sleep studies (HSATs) have clear strengths and some limitations. Knowing both helps you decide whether it’s the right option for your situation.
Benefits
- Privacy and ComfortConducted in your own bedroom, without the feeling of being observed in a lab setting.
- AffordabilityGenerally 70–80% cheaper than a full in-lab polysomnography test.
- Quick ResultsData is uploaded digitally and often reviewed within a few days.
- ConvenienceNo travel, no hospital stay, and no disruption to your daily routine.
Drawbacks
- Limited ScopeHSATs are excellent for diagnosing obstructive sleep apnea, but they may miss complex sleep disorders like narcolepsy, REM behavior disorder, or parasomnias.
- Device Setup IssuesIncorrect placement of sensors can lead to incomplete or inaccurate results.
- Fewer Data PointsUnlike in-lab polysomnography, HSATs don’t typically monitor brain waves, leg movements, or multiple sleep stages in detail.
💬 Pull Quote:
"At-home sleep studies are best suited for patients with suspected obstructive sleep apnea — but they are not a substitute for full polysomnography in complex cases."
How Much Does an At Home Sleep Study Cost?
The cost of an at-home sleep study can vary based on location, provider, and insurance coverage.
- Price Range: Typically $150–$500 per study.
- Lab Study Comparison: A full in-lab sleep study usually costs $1,000–$3,000+.
- Insurance Coverage:
👉 Key takeaway: If your doctor suspects obstructive sleep apnea, an at-home test is usually the most affordable and accessible first step before considering more expensive lab-based studies.
At Home Sleep Study Providers & Devices
Not all at-home sleep tests are the same. The quality of your results depends heavily on whether you use FDA-approved devices and get proper physician guidance.
FDA-Approved Devices:
- WatchPAT – widely prescribed, easy setup, finger-based monitoring.
- ResMed ApneaLink Air – lightweight, tracks airflow, oxygen, and breathing effort.
- Itamar Medical and Nox T3 – advanced devices recommended by sleep clinics.
Telehealth Providers Offering HSAT Kits:
- Many online clinics (such as Lofta, Snap Diagnostics, and regional telehealth networks) ship HSAT kits to your doorstep.
- Patients consult virtually with a sleep physician, then receive a kit, complete the study, and upload results for analysis.
DIY vs. Physician-Prescribed Tests:
- Some companies market “DIY” or direct-to-consumer sleep tests, but not all are FDA-approved.
- Best practice: Choose a physician-prescribed HSAT to ensure accurate results, insurance coverage, and proper follow-up treatment.
At Home Sleep Study Success Stories
Hearing from real patients makes the benefits of HSATs clearer.
Testimonial #1 (Conversational Style):
“I was snoring so loudly my partner begged me to get checked. I didn’t want to spend a night in the hospital, so my doctor suggested a home sleep test. It was simple to set up. A week later, I had a diagnosis of sleep apnea, started CPAP, and now I wake up refreshed.”
Testimonial #2 (Reddit-Friendly Story):
“I thought I was just tired from work. But after my at-home sleep study, I found out I stopped breathing 20+ times an hour. Now I use CPAP, and my blood pressure is down, and I’m not falling asleep at my desk anymore.”
Case Study:
- Patient: 48-year-old male, BMI 32, hypertension, loud snoring.
- Process: Telehealth physician prescribed HSAT → Diagnosis of moderate obstructive sleep apnea (AHI: 22 events/hour).
- Treatment: CPAP therapy + weight management program.
- Outcome: Better sleep quality, reduced daytime fatigue, improved blood pressure control.
Common Myths About At Home Sleep Studies
Many misconceptions stop people from considering HSATs. Let’s clear them up:
“They’re less accurate than lab tests.”
- ❌ Myth: HSATs can’t provide reliable results.
- ✅ Fact: For obstructive sleep apnea, HSATs are often just as accurate as in-lab studies. The difference is in complexity—lab studies are needed for less common sleep disorders.
“Anyone can order one without a doctor.”
- ❌ Myth: You can just buy a kit online without oversight.
- ✅ Fact: In many regions, HSATs require a doctor’s prescription. Direct-to-consumer kits exist, but physician-prescribed tests ensure proper diagnosis and insurance coverage.
“It’s uncomfortable to wear the device.”
- ❌ Myth: You’ll be tangled in wires all night.
- ✅ Fact: Modern HSAT devices are lightweight, wireless, and user-friendly, designed for minimal disruption while you sleep.
👉 Key takeaway: At-home sleep studies are trusted medical tools, not gimmicks. With FDA-approved devices, physician oversight, and simple technology, they offer a safe, reliable, and convenient way to diagnose sleep apnea.
At Home Sleep Study Alternatives
If you’re not ready for a physician-prescribed HSAT, there are a few alternatives—but they come with limitations.
- Wearable Sleep Trackers (Fitbit, Oura Ring, Apple Watch):
- Overnight Oximetry Tests:
- Lifestyle Changes:
👉 Takeaway: These alternatives may provide helpful insights or preventative benefits, but if you suspect sleep apnea, an at-home or in-lab sleep study remains the gold standard for diagnosis.
The Future of At Home Sleep Studies
Sleep diagnostics are evolving rapidly, driven by AI, telemedicine, and smart wearables.
AI-Based Sleep Monitoring:
- Machine learning algorithms can analyze sleep data in real time, detecting patterns beyond human scoring.
- AI may help distinguish between different sleep disorders with greater accuracy.
Integration with Telemedicine Platforms:
- Remote consultations and digital result sharing make it easier for patients to get timely care.
- End-to-end digital workflows are reducing wait times for diagnosis and treatment.
Continuous Monitoring Through Smart Wearables:
- Next-gen devices (smart rings, patches, wireless headbands) may allow long-term monitoring instead of just one night.
- Continuous data could help track treatment effectiveness, like how CPAP improves sleep quality over weeks and months.
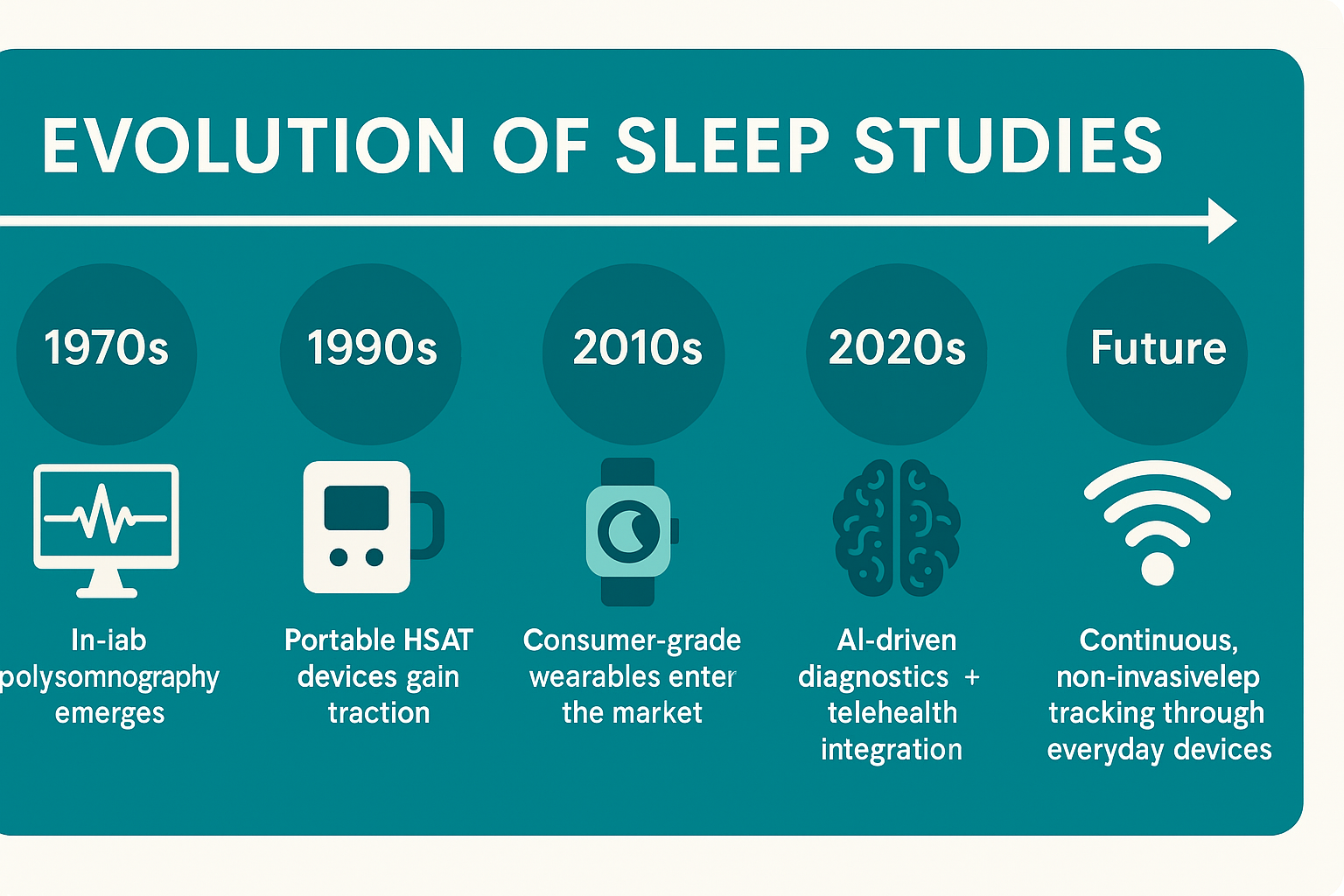
👉 Key takeaway: The future of sleep studies lies in making testing smarter, more accurate, and seamlessly integrated into daily life.
Final Thoughts — Should You Try an At Home Sleep Study?
An at-home sleep study (HSAT) can be a life-changing first step for anyone struggling with loud snoring, daytime fatigue, or suspected sleep apnea.
- Pros: Convenient, private, affordable, and effective for diagnosing obstructive sleep apnea.
- Cons: Limited in scope—may miss complex sleep disorders that require full in-lab polysomnography.
The bottom line?
👉 At-home sleep studies are an excellent starting point for most people with suspected sleep apnea. But they’re not a replacement for comprehensive lab testing when more complex conditions are involved.
Above all, it’s critical to consult a qualified sleep specialist before making decisions based on your results. Only a doctor can interpret your test, recommend treatments like CPAP, and guide next steps if more testing is needed.
✨ Takeaway: Don’t ignore poor sleep—it affects your health, mood, and even heart function. If you suspect a problem, talk to your doctor about whether an at-home sleep study is right for you. Prioritizing your sleep today could protect your long-term health tomorrow.
FAQs on At Home Sleep Study
What is the difference between an at-home sleep study and a lab sleep study?
An at-home sleep study (HSAT) is done in your own bed using a portable device that tracks breathing, oxygen levels, and heart rate. A lab sleep study (polysomnography) is performed in a sleep clinic with advanced monitoring, including brain waves, muscle movement, and detailed sleep stages.
Is an at-home sleep study accurate for sleep apnea diagnosis?
Yes. HSATs are highly accurate for diagnosing obstructive sleep apnea (OSA) but may miss more complex disorders like narcolepsy or parasomnia.
How do I prepare for a home sleep study?
Avoid caffeine and alcohol, follow your normal bedtime routine, wear sensors as instructed, and sleep in your usual position.
Do I need a doctor’s prescription for an at-home sleep study?
In most regions, yes. A doctor’s order ensures accuracy, insurance coverage, and proper interpretation of your results.
How much does an at-home sleep study cost with insurance?
With insurance, most patients pay $0–$150 out-of-pocket. Without insurance, costs typically range from $150–$500, compared to $1,000+ for lab studies.
Can I use my smartwatch as a replacement for a home sleep study?
No. Smartwatches track sleep patterns and oxygen levels but cannot diagnose sleep apnea. They’re useful for screening but not a medical substitute.
What happens after I get my sleep study results?
Your doctor reviews the data and may recommend CPAP therapy, oral appliances, lifestyle changes, or further testing in a lab if needed.
Are home sleep studies safe for children or elderly patients?
Yes, but with caution. HSATs are safe for most adults, but children and frail elderly patients often need lab-based monitoring for more accuracy.
What should I do if my home sleep study is inconclusive?
Your doctor may order a repeat test or a full in-lab polysomnography for a clearer diagnosis.
How long does it take to get results from an at-home sleep study?
Typically 3–7 days, depending on how quickly your device is returned and reviewed by a physician.
Do at-home sleep studies really work?
Yes. They’re widely used and FDA-approved, especially effective for diagnosing obstructive sleep apnea.
How do I do a sleep study at home?
Your doctor prescribes a device, you set it up before bed (finger sensor, chest belt, nasal cannula), sleep as usual, and return/upload the data for review.
Will insurance pay for an at-home sleep study?
Most insurance plans—including Medicare—cover HSATs when prescribed by a doctor.
What is the 4% rule in a sleep study?
It refers to a 4% drop in blood oxygen saturation that’s used to score hypopnea (shallow breathing events) in many sleep studies.
What not to do during a sleep study?
Avoid caffeine, alcohol, daytime naps, and skin lotions (they can interfere with sensors).
What is the 438 sleep method?
It’s a viral TikTok sleep hack suggesting you fall asleep in 4 minutes by focusing on 3 breaths and 8 seconds of calm—but it’s not a medical sleep study method.
How many hours do you sleep during a sleep study?
Aim for at least 6 hours of sleep, but even 4–5 hours can provide useful diagnostic data.
What will make you fail a sleep study?
There’s no “failing,” but improper sensor setup, not sleeping enough, or device malfunction may require a repeat study.
Can I pee during a sleep study?
Yes. For at-home tests, you can disconnect/reconnect sensors briefly. In-lab, technicians assist you without disrupting the test.
Can I nap the day of a sleep study?
Avoid napping. Being naturally tired at bedtime helps ensure accurate results.
Should I wear a bra to a sleep study?
It’s best to wear loose, comfortable sleepwear. A bra is not required and may interfere with chest belts.
What happens if you can’t fall asleep during a sleep study?
Try to relax—some sleep is enough for data collection. If too little data is recorded, your doctor may suggest a repeat test.
What are the mild symptoms of sleep apnea?
Snoring, morning headaches, daytime fatigue, irritability, and waking up gasping for air are common early signs.
How should I wear my hair for a sleep study?
For HSATs, hair usually doesn’t matter. For in-lab studies, wear clean, dry hair without oils or products so sensors stick properly.